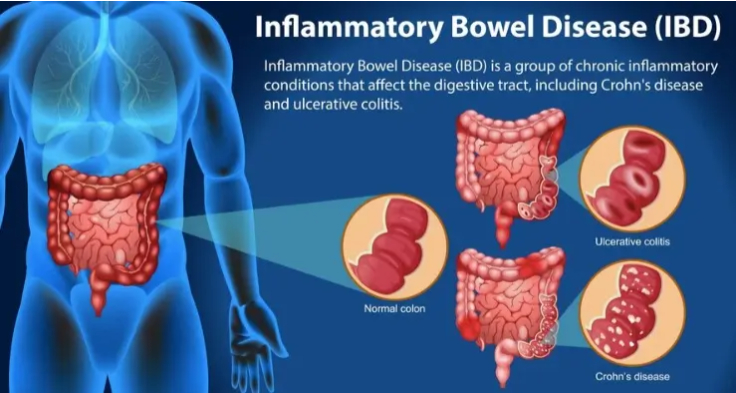
Inflammatory Bowel Disease (IBD) is a term used to describe a group of chronic conditions characterized by inflammation of the gastrointestinal (GI) tract. The two most common forms of IBD are Crohn’s disease and ulcerative colitis, which differ in their specific areas of impact within the digestive system.
IBD is a serious health issue that affects millions worldwide and can significantly reduce quality of life if not managed properly.
Symptoms of Inflammatory Bowel Disease
The symptoms of IBD can vary depending on the severity of the condition and the part of the GI tract affected. Common symptoms include:
- Abdominal pain and cramping: Persistent discomfort or pain in the abdomen.
- Diarrhea: Often severe, sometimes accompanied by blood or mucus.
- Fatigue: Due to inflammation, malnutrition, or anemia.
- Unintended weight loss: A result of decreased appetite or poor absorption of nutrients.
- Fever: Common during flare-ups.
- Rectal bleeding: A symptom particularly associated with ulcerative colitis.
- Reduced appetite: Often due to abdominal pain and nausea.
Causes and Risk Factors
While the exact cause of IBD is unknown, it is believed to result from a combination of factors:
- Immune system malfunction: An overactive immune response may mistakenly attack the cells in the GI tract, causing inflammation.
- Genetic predisposition: Individuals with a family history of IBD are at higher risk.
- Environmental triggers: Certain triggers like diet, smoking, or infections may play a role in initiating or worsening symptoms.
- Microbiome imbalance: Changes in gut bacteria might contribute to the disease’s development.
Risk factors for IBD include age (often diagnosed between 15 and 35 years), ethnicity (more common in Caucasians), and lifestyle factors such as smoking.
Types of Inflammatory Bowel Disease
- Crohn’s Disease:
- Affects any part of the GI tract, from the mouth to the anus.
- Involves all layers of the bowel wall.
- Common complications include fistulas, strictures, and abscesses.
- Ulcerative Colitis:
- Primarily affects the colon and rectum.
- Involves only the innermost lining of the colon.
- Complications can include toxic megacolon and an increased risk of colon cancer.
Diagnosis
IBD is diagnosed through a combination of medical history, physical examination, and diagnostic tests, such as:
- Blood tests: To check for anemia or markers of inflammation.
- Stool tests: To rule out infections and detect inflammation markers.
- Endoscopy/Colonoscopy: Visual examination of the GI tract and biopsy collection.
- Imaging tests: CT scans, MRI, or ultrasound to assess damage or inflammation.
Management and Treatment
IBD is a lifelong condition that requires a tailored treatment approach to manage symptoms and prevent complications. Treatment options include:
- Medications:
- Anti-inflammatory drugs: Such as aminosalicylates and corticosteroids.
- Immune system suppressors: Like azathioprine or biologics (e.g., infliximab).
- Antibiotics: For managing infections related to Crohn’s disease.
- Symptomatic relief medications: Antidiarrheal agents and pain relievers.
- Dietary and Lifestyle Changes:
- Eating a balanced diet tailored to individual triggers.
- Avoiding high-fat and high-fiber foods during flare-ups.
- Maintaining hydration and considering supplements like iron or calcium.
- Surgery:
- Necessary for cases that do not respond to medication.
- For Crohn’s disease, it may involve removing affected portions of the GI tract.
- For ulcerative colitis, a colectomy (removal of the colon) may be curative.
- Psychological Support:
- IBD is linked to stress and mental health issues; counseling or support groups can be helpful.
Living with IBD
Managing IBD requires a holistic approach, including regular follow-ups with healthcare providers, adherence to treatment plans, and a focus on overall well-being. Advances in treatment, including biologics and personalized medicine, are improving outcomes and quality of life for those with IBD.
For anyone experiencing persistent digestive symptoms, early diagnosis and intervention are key to effectively managing IBD and minimizing its impact on daily life.