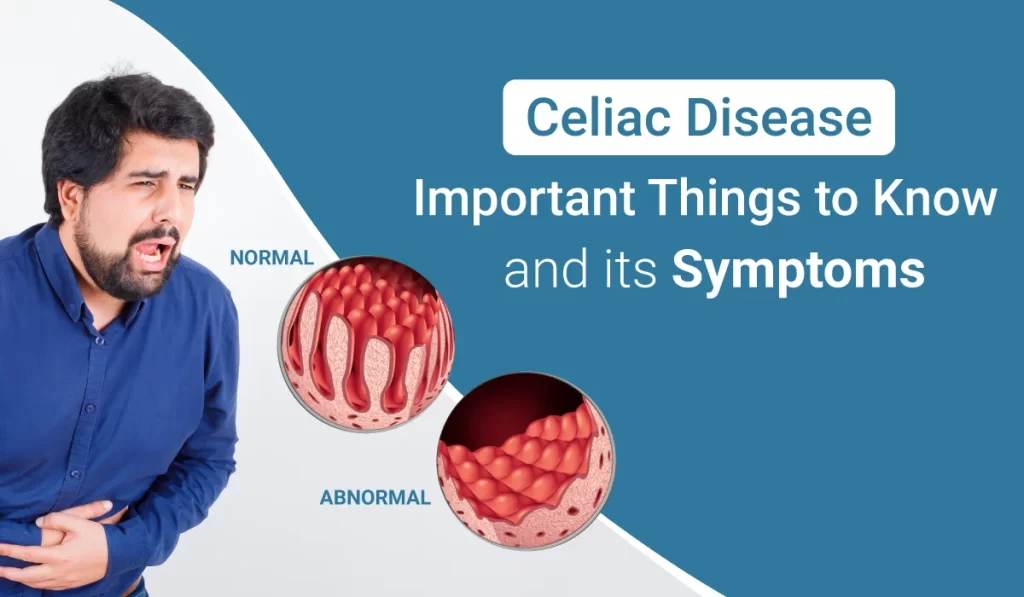
Celiac disease is a chronic autoimmune disorder that primarily affects the small intestine, occurring in genetically predisposed individuals. It is characterized by a severe intolerance to gluten, a protein found in wheat, barley, rye, and derivatives of these grains. When people with celiac disease consume gluten, their immune system responds by damaging the villi of the small intestine.
Villi are tiny fingerlike protrusions that play a critical role in nutrient absorption. Damaged villi impair the body’s ability to absorb nutrients properly, leading to malnutrition and a variety of gastrointestinal and non-gastrointestinal symptoms.
Symptoms
Celiac disease can present a wide range of symptoms, which vary significantly among individuals. Some people may experience severe symptoms, while others may have none at all, despite having damage to their small intestine. Common symptoms include:
- Digestive problems (abdominal bloating, pain, gas, diarrhea, pale stools, and weight loss)
- A severe skin rash known as dermatitis herpetiformis
- Iron-deficiency anemia
- Musculoskeletal problems (muscle cramps, joint and bone pain)
- Growth problems and failure to thrive in children
- Neurological symptoms (fatigue, headache, depression, anxiety, and peripheral neuropathy)
Diagnosis
The diagnosis of celiac disease involves several steps, including serological (blood) tests to look for elevated levels of certain autoantibodies and an endoscopic biopsy of the small intestine to observe the degree of villus atrophy. Genetic testing may also be performed to identify human leukocyte antigens (HLA-DQ2 and HLA-DQ8) that are almost universally present in patients with celiac disease. However, the presence of these genes alone does not confirm the disease, as they are also found in a portion of the general population without the disease.
Treatment
The primary treatment for celiac disease is a strict, lifelong gluten-free diet, which helps heal intestinal damage and alleviate symptoms. Following a gluten-free diet requires significant dietary changes and vigilance, as gluten is a common ingredient in many foods. Patients are advised to avoid all products containing wheat, barley, rye, and their derivatives. Oats may be included in the diet but must be certified gluten-free to avoid cross-contamination.
In addition to dietary management, individuals with celiac disease may need nutritional supplements to correct deficiencies (e.g., iron, calcium, vitamin D) until their intestine heals. It’s also important for patients to work closely with a healthcare team, including a doctor who specializes in celiac disease and a dietitian who can provide education and support for managing the diet.
Epidemiology and Risk Factors
Celiac disease affects people worldwide, with varying prevalence rates. It is most common in individuals of European descent but can occur in any ethnic group. Risk factors for developing celiac disease include having a first-degree relative with the disease, having type 1 diabetes, Down syndrome, Turner syndrome, and autoimmune thyroid disease.